Compression Therapy
Compression therapy consists of stockings, panty hose, bandages and other devices that exert compression on your legs for the purpose of improving circulation. It is the most conservative treatment option to alleviate the symptoms of venous insufficiency and to retard the progression of the disease.
Properly fitted gradient compression stockings provide 20-30, 30-40 or 40-50 mm HG of compression at the ankle, with gradually decreasing compression at more proximal levels of the leg. This amount of gradient compression is sufficient to restore normal venous flow patterns in many or most patients with superficial venous reflux and to improve venous flow, even in patients with severe deep venous incompetence. The degree of compression will vary depending on your specific condition.
Compression is also used as adjuvant treatment to enhance the effectiveness of other treatment modalities. Most patients with symptoms due to venous insufficiency can benefit from the effects of gradient compression hose.
Sclerotherapy
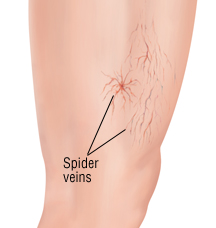
Sclerotherapy consists of injecting a medical solution into a target vein which causes it to shrink and then dissolve over a period of weeks. Sclerotherapy has been employed in the treatment of varicose veins for over 150 years and treatments have evolved during that time. Modern techniques include ultrasound guidance and foam sclerotherapy.
Sclerotherapy is a non-invasive procedure in which a sclerosant solution is injected into the abnormal surface veins. The patient’s leg is then compressed with either stockings or bandages The procedure takes only about 10 to 15 minutes to perform with minimal downtime Sclerotherapy it is considered the “gold standard” and is preferred over laser for eliminating spider and varicose leg veins. Unlike a laser, the sclerosing solution additionally closes the “feeder veins” under the skin that are causing the spider veins to form, thereby making a recurrence of the spider less likely.
Sclerotherapy can also be performed using “foamed sclerosant drugs” under ultrasound guidance to treat larger varicose veins. After a map of the patient’s varicose veins is created using ultrasound, these veins are injected whilst real-time monitoring of the injections is undertaken, also using ultrasound. The sclerosant can be observed entering the vein, and further injections performed so that all the abnormal veins are treated. Follow-up ultrasound scans are used to confirm closure of the treated veins, and any residual varicose veins can be identified and treated.
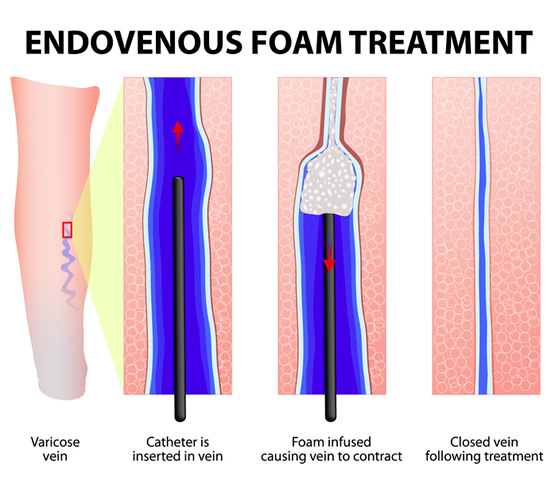
Microfoam
This is an FDA-approved chemical ablation treatment option for trunk vein reflux. The microfoam solution is prepared to produce a consistent foam for injection. The foam state of the sclerotherapy medication improves its effectiveness for closing the vein. As with all ablations, the goal is to close the trunk vein that is refluxing. This should improve the symptoms of venous incompetence and prevent progression of disease. This form of treatment does not require local anesthesia to prepare the vein.
During this procedure, foam sclerosant will be injected into the target vein using a small catheter. The microfoam fills the section of the vein being treated and causes a chemical injury to the wall of the vein resulting in contraction of the vein and eventual closure. Blood flow will shift to healthier veins as a result.
Our doctors will determine if you are a good candidate for this method. It is virtually pain free and requires only minimal local anesthetic at the injection site. Recovery time is minimal and most activities can be resumed the same day. Patients must wear compression hose after treatment. As with all vein treatments, there is a risk of blood clots and/or allergy with the use of sclerosant.
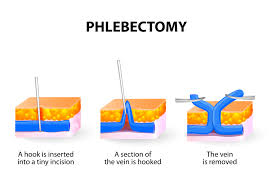
Minimal Phlebectomy
Minimal phlebectomy is a technique to remove varicose veins through tiny punctures or minimal skin incisions. It is indicated for the treatment of bulging varicosities that would not respond well to sclerotherapy due to their thickness. Robert Muller, a Swiss dermatologist is largely responsible for its’ worldwide popularity. The procedure is performed under local anesthesia in the Optima Vein Care office. Phlebectomy hooks are used to extract the varicose veins through small incisions assuring complete and definite eradication of the veins. The small size of the skin incisions requires no sutures and usually results in little or no scarring. Normal daily activities are resumed immediately, except for strenous exercise. Following the procedure patients will have bandages applied and they will wear compression hose continually for 3 days, then for 10 days only during the day.
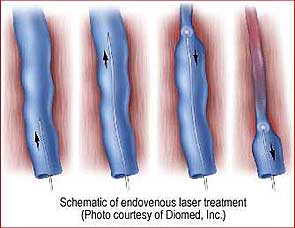
Endoveneous Laser Abation (EVLT)
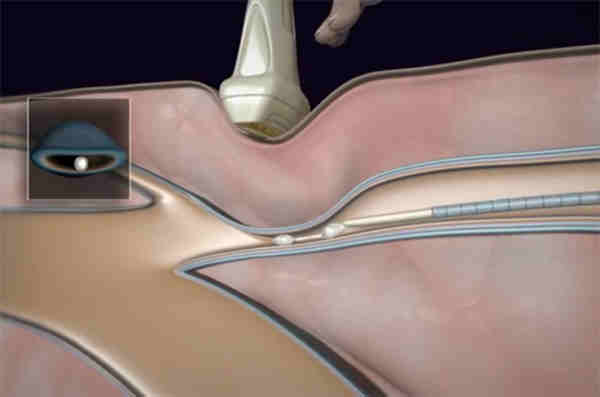
Endovenous Laser Therapy is used to treat reflux induced venous insufficiency of the great and short saphenous veins as well as other selected veins. EVLT is an ambulatory minimally-invasive procedure. Initially, a small laser fiber is threaded through the length of the abnormal vein to be treated. Then, as this fiber is slowly withdrawn, the laser is fired delivering thermal energy (heat) to the vein walls. The induced localized damage causes the vein to close and disappear.
FDA approved in 2002, the use of EVLT has increased rapidly due to the numerous advantages it brings over the traditional vein stripping procedure. A prominent study in the Journal of Vascular and Interventional Radiology showed a better than 93% success rate after two years. These results are comparable or superior to other methods for treating varicose veins, including surgery, with lower complication rates while avoiding general anesthesia.
VenaSeal® Sapheon Closure System
VenaSeal® offers a minimally invasive treatment option that uses an advanced medical adhesive to seal the diseased vein.
The procedure is performed in a doctor’s office or clinic under local anesthetic only. A small catheter is inserted into the diseased vein and small amounts of adhesive are delivered through the catheter until the entire vein segment is sealed.
The entire procedure takes less that one hour.
After the procedure, a small bandage will be placed at the vein access site. Most patients are able to return to normal actives immediately after the procedure.
The procedure was FDA approved in February 2015 and is currently covered by Medicare.
MOCA (ClariVein)
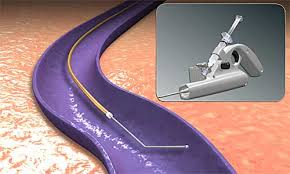
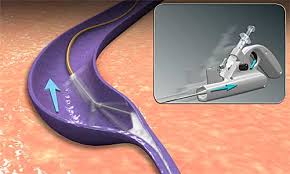
MOCA varicose vein treatment using the patented ClariVein catheter is a new endovascular technique for the treatment of venous reflux disease.
It is the first venous ablation technique to employ a hybrid (dual-injury) technique built into 1 catheter-based delivery system.
- Endomechanical abrasion of the vessel endothelia is produced by the tip of the catheter’s rotating wire (mechanical component).
- Endovenous chemical ablation is induced simultaneously by the injection of a sclerosant drug sprayed from the tip of the catheter as it is pulled back.
The procedure with ClariVein is minimally invasive and takes less than 30 minutes and has several benefits, including minimal patient discomfort during and after the procedure.
As the procedure is relatively recent, insurance coverage may not be available.