


Conveniently book your appointment with us today. Feel free to complete our registration forms prior to your visit. We look forward to serving you!
Dr. Paul Sos, M.D., is the founder of Optima Vein Care. He received training in Phlebology at the European School of Phlebology and was one of the first physicians to become Board Certified in Phlebology. His professional experience encompasses twenty years in the diagnosis and treatment of venous disease.
BBA: University of Texas at El Paso
Medical Degree: University of Paris VII
Appointments: Radiology Attache Xavier-Bichat Hospital (Paris)
Credential: Registered Vascular Technologist (ARDMS)
Board Certified Diplomat: American Board of Venous and Lymphatic Medicine(ABVLM) – formally the American Board of Phlebology (ABPh)
Board Certified: American Board of Family Medicine
Member: American College of Phlebology
On staff at:
Banner Estrella Hospital
Dignity Health: Chandler Regional Hospital
Dignity Health: Mercy Gilbert Hospital Scottsdale Healthcare Thompson Peak
Kylee Brennan, PA-C, is a Board Certified Physician Assistant providing advanced, minimally invasive vein care to patients at Optima Vein Care. A lifelong Arizona resident, Kylee was born and raised in Scottsdale and is proud to serve the community she calls home.
Before joining Optima Vein Care, Kylee gained extensive experience in Interventional Radiology at a major hospital, where she specialized in performing image-guided procedures, including port placements and venous access. Her background in radiology and procedural care has equipped her with the skills and precision needed for today’s leading-edge vein treatments.
Kylee earned her Bachelor of Science in Physiology from the University of Arizona and went on to complete her Master of Physician Assistant Studies at Touro University Nevada. She is board certified by the National Commission on Certification of Physician Assistants and is a member of the American Academy of Physician Assistants.
With a commitment to delivering compassionate, high-quality care, Kylee combines clinical expertise with a personal approach to help patients feel comfortable, informed, and confident throughout their treatment journey.
With over 30 years of experience in general, vein, and skin surgery, Thomas McCrorey, MD, CHCQM, is joining Optima Vein Care in spring 2025. Dr. McCrorey grew up all over the country as a “military brat,” but his family has lived in the West for over 100 years.
After graduating from college, Dr. McCrorey joined the military himself. Following three years in combat positions for the U.S. Army, he earned his Doctor of Medicine from the Uniformed Services University of the Health Sciences in Bethesda, Maryland, and completed his residency in General Surgery in 1998. He spent much of his medical career in the military and is board certified in General Surgery, including vein disorders.
In his general surgical practice, Dr. McCrorey provided surgical care and medical leadership at sea, in Afghanistan and Iraq, as well as in multiple military and civilian hospitals. After completing surgical residency, he received additional training and experience in state-of-the-art vein procedures, ultrasound, and cosmetic and medical skin care.
He also earned certification in Quality Assurance and, for several years, helped the state of Nevada improve quality healthcare for underserved residents. For the last five years, he has focused his clinical practice on minimally invasive vein care and continues to serve the nation as a doctor in the Air National Guard.
Spider veins are tiny red, blue or purple veins that commonly appear on the surface of the thighs, calves and ankles. They tend to take on one of three characteristic patterns; a “sunburst” or spider-web pattern radiating outward from a central point, a “tree-branch” pattern, or a “matting” or linear pattern that may be nothing more than a set of thin lines.
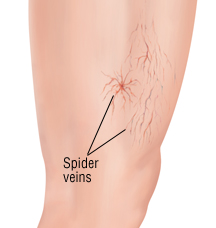
Spider veins are extremely frequent and may be associated with symptoms such as burning and itching or just an uncomfortable feeling in the legs. Risk factors for spider veins are similar to those for varicose veins; age, heredity, pregnancy, hormonal changes, obesity and extended periods of standing as well as sun exposure and injuries to the skin surface.
Spider veins may be isolated or associated with “feeder” veins or with larger underlying varicose veins. They are often considered merely cosmetic, but can signal an abnormal increase in pressure in the venous system in the legs. For that reason, most physicians prefer to conduct an ultrasound exam to determine the extent of the problem and the underlying causes of the condition before formulating a treatment plan. Contact us for more info on spider vein treatment in Phoenix, Chandler and Scottsdale, Arizona.
Dr. Frank Bonavita, M.D., F.A.C.C., completed his undergraduate studies at Brown University. He earned his medical degree in 1979 from the University of Cincinnati College of Medicine. He went on to complete his Internship, Residency and Fellowship training in Cardiovascular Diseases at the Cornell University teaching hospitals in New York.
Dr. Bonavita is Board Certified in Internal Medicine and Cardiovascular Disease. He is a Fellow of the American College of Physicians and a Fellow of the American College of Cardiology. He served as a Chairman of the Department of Cardiology and Director of the Cardiac Catheterization Laboratory at St. Jude Medical Center in Fullerton, CA for over ten years.
He specializes in the treatment of varicose vein disease and venous insufficiency and is a member of the American College of Phlebology.
Dr. Robert David Stoffey, DO, ABVLM, RVT, RPhS, RVS, DABR, DAOBR, CAQ-Neuroradiology is a board-certified physician providing state-of-the-art, total vein care to patients in the Greater Scottsdale Metroplex. Dr. Stoffey graduated with honors from the Western University of Health Sciences, College of Osteopathic Medicine, located in Pomona, California, just prior to embarking on a career with the US Army Medical Corps, where he served overseas in both West Germany and the Republic of Korea. During his military service, Dr. Stoffey held a number of leadership and administrative roles. He completed a transitional internship at Fitzsimons Army Medical Center in Denver as well as a diagnostic radiology residency in San Antonio. Since leaving the military, Dr. Stoffey has completed three radiology imaging fellowships, the most recent being in neuroradiology with an emphasis on venous and vascular interventional procedures at the University of Texas in Houston.
Dr. Stoffey is certified by the American Board of Venous and Lymphatic Medicine as well as holding lifetime, board-certification by both the American Board of Radiology and the American Osteopathic Board of Radiology in diagnostic radiology; additionally, he holds a certificate of added qualification in neuroradiology from the AOBR. Dr. Stoffey also holds certifications in the following disciplines: RVT (Registered Vascular Technologist), RPhS (Registered Phlebology Sonographer), and RVS(Registered Vascular Specialist).
Dr. Stoffey is an active member of the American Vein & Lymphatic Society. He is an active member of the American Roentgen Ray Society, an internationally-recognized medical society dedicated to research, education, and treatment of medical imaging. Dr. Stoffey is an article reviewer for the peer-reviewed journal, the American Journal of Roentgenology. Dr. Stoffey is also a book reviewer for the peer-reviewed journal Radiology. Dr. Stoffey has performed an extensive amount of medical research, to include having authored peer-reviewed material. He has spoken numerous times, as an invited speaker, at both medical conferences as well as to civic and community groups, both regionally and nationally. Dr. Stoffey holds unrestricted medical licenses in fifteen U.S. states. Dr. Stoffey has had extensive training in state-of-the-art venous interventions.
Regarding his personal interest in treating chronic venous insufficiency and the entire spectrum of venous and lymphatic disorders, Dr. Stoffey describes his professional ambitions as both timely and needed as an estimated 45 million Americans are experiencing chronic venous insufficiency. This spectrum of disorders, felt to be widely under-recognized and even more so under treated, affects a large segment of the American population; due mainly but not limited to obesity, occupational demands, diabetes, lymphedema, a lack of exercise, as well as an aging population.
Dr. Stoffey has been utilizing medical ultrasonography – the main diagnostic imaging tool to assess venous disease – since 1994; additionally, Dr. Stoffey has been trained in and has been performing interventional venous procedures, also since 1994. Being able to diagnose, treat, and follow up a patient with chronic venous insufficiency on an ongoing basis is extremely rewarding to Dr. Stoffey’s professional aspirations, as he states “I have long enjoyed performing venous interventional procedures, and here at Optima Vein Center, I am able to follow my patients from their initial office visit through all minimally-invasive treatments and finally with follow up visits. The continuity of care that I provide at Optima is essential to the successful treatment of my patients.”
By providing state-of-the-art vein care treatment –in an outpatient office setting – for varicose veins and associated venous pathology to my patients using minimally-invasive techniques is exactly what my patients are seeking. My patients can receive the best available treatment for their veins without the need to visit a hospital. While venous disease is poorly understood by many physicians, the doctors at the Optima Vein Care have a sound fundamental knowledge of venous disease, it’s treatment, and appropriate follow up care – in fact, it’s our area of subspecialization – we treat only adults, we treat only veins and we treat only legs. Our patients are extremely satisfied with the professional level of treatment and outcomes that they receive from Optima Vein as we specialize in total vein care, which includes not only medically-indicated chronic venous reflux, but also aesthetic treatments of spider veins and varicose veins. Following our advanced vein treatments, patients can rapidly resume normal activities and almost immediately they notice a significant improvement in their quality of life.
Dr. John Opie, M.D., is recognized for his innovative work in the treatment of deep venous insufficiency (DVI), which can result from deep venous blood clots and lead to leg ulcerations. He has been published in many peer reviewed journals and is the inventor of the “Monocusp” procedure, for the management of DVI. He is the Editor-in-Chief of an soon to be published medical text book: Pulmonary Embolism. As an avid inventor, he currently holds 22 patents for various medical devices. He is also an author and has 5 novels published. He has been practicing Cardiothoracic and Vascular Surgeryin Phoenix since 1991.
Medical Degree: New Zealand (MD)
General Surgical Residency: London, England (National Heart & Brompton Hospital) FRCS
Cardiothoracic Surgical Training: Vancouver, British Columbia (Vancouver General and BC Children’s Hospitals) FRCS(C)
Board Certified: General Surgery, Vascular Surgery and Cardiothoracic Surgery
Appointments: Associate Professor in Cardiovascular and Thoracic Surgery at the University of British Columbia
Varicose veins can predispose to the formation of both superficial and deep venous clots or thrombosis . Deep venous thrombosis (DVT) mainly forms in the large veins in the legs. The clot can block blood flow and cause swelling and pain. A blood clot can also break free in the legs and travel to the lungs (pulmonary embolus), and can be life-threatening. Rapid treatment of DVT helps prevent this problem.
Symptoms of blood clots can include; increased warmth, pain or tenderness in one leg, skin that feels warm or tender to the touch or just swelling. Rapid evaluation by a health care provider is imperative if you have symptoms of a DVT.
Varicose veins are the visible surface manifestation of an underlying condition called venous insufficiency. When blood does not flow properly from the surface veins to the deep veins, pressure can build up causing loosely supported superficial veins to become dilated and twisted. Those lying in the fat under the skin give rise to varicose veins which can vary in size from quite small (2-3mm across) to very large (2-3 cm across).
Very small veins are called “spider veins” or “thread veins”. These veins are different from varicose veins because they are situated within the layer of the skin itself. They may look like short, fine lines, “starburst” cluster, or web-like maze. Spider veins are most common on the thighs, ankles and feet.

Vein failure leads to abnormally high pressure in the leg veins which can force fluid out into the tissues causing swelling (edema). High vein pressures and stress on the vein walls also leads to red and white blood cells being forced or migrating out of the blood vessels into the tissues. When this occurs over an extended period of time, venous insufficiency can cause a number of skin problems.
As red blood cells break down their iron is deposited in the tissues leading to a brown discoloration (skin pigmentation). As activated white blood cells enter the tissues they release chemicals that damage the tissues. This may lead to the build up of products (e.g. fibrin) that impede diffusion of oxygen and other nutrients. The first skin signs are often mild eczema with wet and itchy, red scaly skin (varicose eczema), usually just above the ankle. More advanced skin lesions appear as shiny white areas of skin (atrophie blanche) or include hardening of the fatty layer beneath it (lipodermatosclerosis).
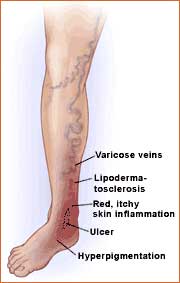
The ultimate result can be death of the tissues surrounding the veins leading to ulceration (venous stasis ulcers). The typical venous ulcer occurs on the lower leg (usually near the ankle where the vein pressures are highest) and is often surrounded by skin having a rusty brown color.
