Dr. Robert David Stoffey, DO, ABVLM, RVT, RPhS, RVS, DABR, DAOBR, CAQ-Neuroradiology is a board-certified physician providing state-of-the-art, total vein care to patients in the Greater Scottsdale Metroplex. Dr. Stoffey graduated with honors from the Western University of Health Sciences, College of Osteopathic Medicine, located in Pomona, California, just prior to embarking on a career with the US Army Medical Corps, where he served overseas in both West Germany and the Republic of Korea. During his military service, Dr. Stoffey held a number of leadership and administrative roles. He completed a transitional internship at Fitzsimons Army Medical Center in Denver as well as a diagnostic radiology residency in San Antonio. Since leaving the military, Dr. Stoffey has completed three radiology imaging fellowships, the most recent being in neuroradiology with an emphasis on venous and vascular interventional procedures at the University of Texas in Houston.
Dr. Stoffey is certified by the American Board of Venous and Lymphatic Medicine as well as holding lifetime, board-certification by both the American Board of Radiology and the American Osteopathic Board of Radiology in diagnostic radiology; additionally, he holds a certificate of added qualification in neuroradiology from the AOBR. Dr. Stoffey also holds certifications in the following disciplines: RVT (Registered Vascular Technologist), RPhS (Registered Phlebology Sonographer), and RVS(Registered Vascular Specialist).
Dr. Stoffey is an active member of the American Vein & Lymphatic Society. He is an active member of the American Roentgen Ray Society, an internationally-recognized medical society dedicated to research, education, and treatment of medical imaging. Dr. Stoffey is an article reviewer for the peer-reviewed journal, the American Journal of Roentgenology. Dr. Stoffey is also a book reviewer for the peer-reviewed journal Radiology. Dr. Stoffey has performed an extensive amount of medical research, to include having authored peer-reviewed material. He has spoken numerous times, as an invited speaker, at both medical conferences as well as to civic and community groups, both regionally and nationally. Dr. Stoffey holds unrestricted medical licenses in fifteen U.S. states. Dr. Stoffey has had extensive training in state-of-the-art venous interventions.
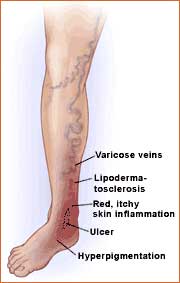
Regarding his personal interest in treating chronic venous insufficiency and the entire spectrum of venous and lymphatic disorders, Dr. Stoffey describes his professional ambitions as both timely and needed as an estimated 45 million Americans are experiencing chronic venous insufficiency. This spectrum of disorders, felt to be widely under-recognized and even more so under treated, affects a large segment of the American population; due mainly but not limited to obesity, occupational demands, diabetes, lymphedema, a lack of exercise, as well as an aging population.
Dr. Stoffey has been utilizing medical ultrasonography – the main diagnostic imaging tool to assess venous disease – since 1994; additionally, Dr. Stoffey has been trained in and has been performing interventional venous procedures, also since 1994. Being able to diagnose, treat, and follow up a patient with chronic venous insufficiency on an ongoing basis is extremely rewarding to Dr. Stoffey’s professional aspirations, as he states “I have long enjoyed performing venous interventional procedures, and here at Optima Vein Center, I am able to follow my patients from their initial office visit through all minimally-invasive treatments and finally with follow up visits. The continuity of care that I provide at Optima is essential to the successful treatment of my patients.”
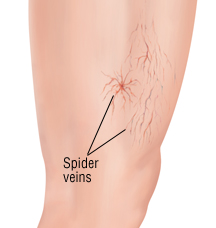
By providing state-of-the-art vein care treatment –in an outpatient office setting – for varicose veins and associated venous pathology to my patients using minimally-invasive techniques is exactly what my patients are seeking. My patients can receive the best available treatment for their veins without the need to visit a hospital. While venous disease is poorly understood by many physicians, the doctors at the Optima Vein Care have a sound fundamental knowledge of venous disease, it’s treatment, and appropriate follow up care – in fact, it’s our area of subspecialization – we treat only adults, we treat only veins and we treat only legs. Our patients are extremely satisfied with the professional level of treatment and outcomes that they receive from Optima Vein as we specialize in total vein care, which includes not only medically-indicated chronic venous reflux, but also aesthetic treatments of spider veins and varicose veins. Following our advanced vein treatments, patients can rapidly resume normal activities and almost immediately they notice a significant improvement in their quality of life.
Click to See Dr Bonavita’s Full CV